By Jeffrey Halbstein-Harris
Right Care Raleigh Chapter Leader
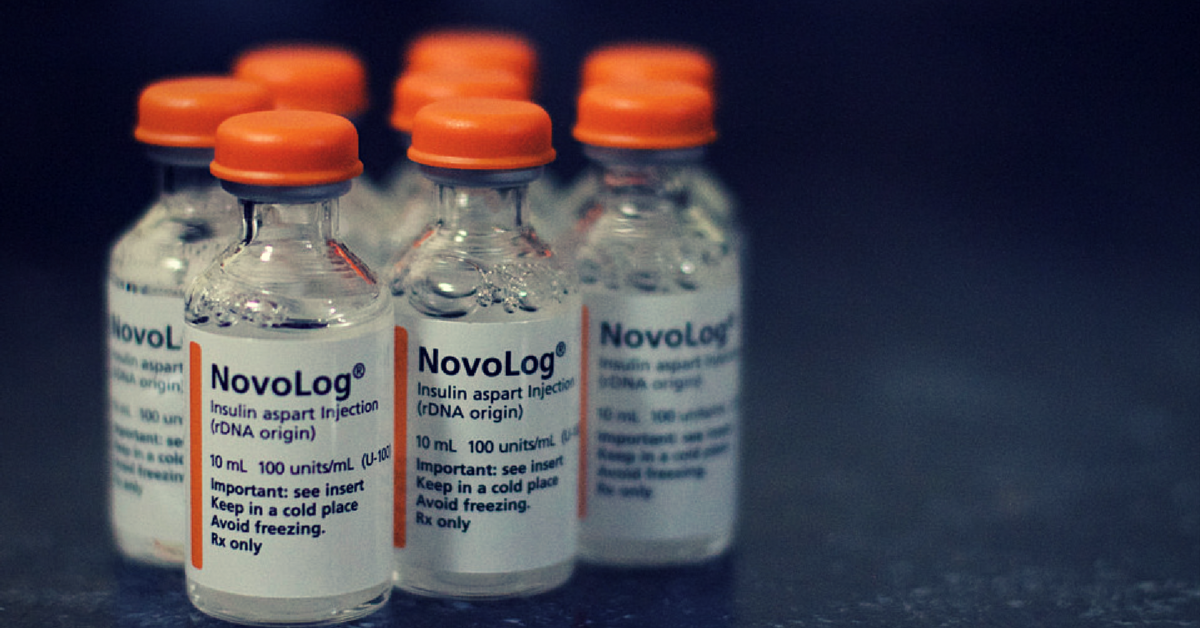
As I was shopping at my local pool store a few weeks ago, making my way through a rack of gaskets to repair our broken pool-pump, a man tapped me on my back and said, “Hey there, do you like that Novalog?” That’s a weird question, I thought? How many times a day does somebody question you about your choice of insulin products?
How many times a day does somebody question you about your choice of insulin products?
Looking up I was met by a smiling, bearded man, perhaps ten or fifteen years my junior, who introduced himself to me as “Mac.” Evidently he had noticed the insulin pen I carry in my shirt pocket to treat “highs” or cover a meal if I chose to eat while I am out. I told Mac that I like Novolog and it works well, but there’s about a 20-minute time lag, so I need to make sure I time it properly.
“Yeah, me too,” said my new found “sugar-brother.” “Unfortunately I am out of it right now and trying not to eat much until pay-day. Last night when I got home my blood sugar was 546. I don’t understand it cause I did nothing but drink water all day.”
I imagine the look on my face startled Mac because he grimaced and said, “Are you alright?” I tried to control my facial expressions but I don’t have a very good poker face.
“Sorry,” I stammered, “What did you do about the high sugar?”
“Well, I didn’t eat dinner, took a boat-load of long acting insulin cause that’s all I have right now, and my sugar was down to the 200s this morning,” said Mac, “ I feel like crap, my head hurts, my vision is blurry and I can’t get enough to drink when I am like that. My wife is really worried about me.”

Mac went on to tell me that he lost his last job unexpectedly and couldn’t afford COBRA insurance, a short-term insurance plan. He was not eligible for coverage under Obamacare in North Carolina because his income fell below the Federal Poverty Level. He should have been eligible for Medicaid, but unfortunately, North Carolina is one of eighteen States that did not accept federal funding to expand Medicaid. Mac is one of many people in this country with chronic illness and low income who are slipping through the cracks.
Mac is one of many people in this country with chronic illness and low income who are slipping through the cracks.
Mac said he would be covered in 90 days and had been “getting by” on insulin samples from his primary care clinic. The clinic supplies are modest and they are only able to dispense two bottles every six weeks or so. The insulin they give him varies in type, so he is constantly changing his dose and schedule, but never feels well because his blood sugar levels are all over the map. To maintain good control of his blood sugar Mac needs four bottles per month, which runs about $750 if purchased online from a discount pharmacy warehouse.
Mac had been stretching his supply by taking less insulin than prescribed and not eating. This means he frequently experiences prolonged periods of high blood sugar and he most certainly is experiencing the symptoms of ketoacidosis; a metabolic reflex to low insulin supply that ultimately causes the diabetic to lapse into coma if it goes untreated. Fortunately, Mac manages to pull himself out “just in the nick of time.” This is an extremely dangerous practice; at least three people with type 1 diabetes died last year from doing exactly what Mac is doing.
At least three people with type 1 diabetes died last year from doing exactly what Mac is doing.
As a type 1 diabetic myself since the age of ten, I find it inconceivable that a nation as wealthy as ours can let people go without the medicine they need to stay healthy and functional. We are often left to our own devices to survive and quite frankly barely cling to life. It is necessary for every person with diabetes or any other chronic illness to master the methods of acquisition and I find myself spending many hours teaching others these “survival skills.”
First things first though – I wanted my new friend to feel better, so I rushed home that evening and returned to the store with a few extra insulin pens (prefilled syringes). Mac was unaware of the Patient Assistance Programs (PAP) that are available through several insulin manufacturers so I gave him the contact information. He applied and found out that he meets the economic qualification requirements; he will receive his insulin in 10-14 days. He had to get to his doctor immediately who was required to complete a bunch of paperwork and write prescriptions. To bridge the gap I gave Mac enough insulin to get through until he receives the first shipment from the manufacturer. His employer’s insurance plan will cost him $600 per month and his insulin will then cost him $180 per month for the co-pays on the 3-4 bottles he requires. Once he has insurance he will no longer qualify for the prescription assistance program.
I am not sure if it’s better for Mac to get insurance or stay on the PAP program. The problem of course is the fact that the PAP program only covers one year of product then comes to a grinding halt. Folks like Mac who live on an income of $1800 per month and whose employers are providing coverage are expected to pay one third or more of their income on insurance and co-pays. Tax breaks for premiums can only do so much – it’s the drug prices that are the problem.
Tax breaks for premiums can only do so much – it’s the drug prices that are the problem.
I have spent no less than $10,000 per year for my health care since the 1990s. Being diagnosed with diabetes in 1966 I count my blessings that I was able to afford my care. Roughly one in ten people in North Carolina has diabetes: that makes 1.27 million of us who are in the same boat.
Until we have real transformative policy change, we are going to have to support each other to get by – what I call the Peer Support Principle. I encourage all persons who have diabetes and are blessed with adequate resources to scratch up a few extra units of their insulin supply and share it with those who do not have enough medicine.
Is this scamming the system? After all, I am taking insulin that my insurance company paid for and sharing it with another person when I have an excess supply at the end of the month. What’s a few units between friends, I ask? “Hey buddy, got an extra dose?”